All In for Virtual Visits
Deck
Working together helps team get ahead of curve
After learning more than a year ago that patients were having trouble getting doctors’ appointments, members of the Keizer Station Family Medicine team in Oregon began exploring ways to improve service and access. Their solution? Offer more video visits.
“What we didn’t realize at the time is that this work would put us in a unique position to be ready for the pandemic, which wasn’t on anyone’s radar in fall 2019,” says Ruthie Berrell, medical office director and management co-lead for the Family Medicine/Nurse Treatment Center unit-based team.
Collaboration by the team’s frontline workers, managers and physicians has served as a partnership model for UBTs in the Northwest Region. It’s also earned the department applause for improving service and access at a critical time in health care, as teams across the enterprise adapt to the rise of virtual care.
“It wasn’t always easy,” says Molly Maddox, RN, the team’s labor co-lead and OFNHP member. “This took a lot of working out the kinks and working together.”
Overcoming resistance to change
One of the team’s earliest challenges involved staff resistance to virtual care. Worried that patients would perceive virtual visits as a “takeaway,” some staff members pushed back.
“The culture of how we delivered care was in the medical office, and people had different levels of acceptance across the spectrum,” says Caroline King-Widdall, MD, team co-lead and physician in charge.
So, team members educated their peers on the benefits of virtual care and developed scripting to help them feel at ease offering video appointments to patients.
“People are more comfortable now taking the lead and scheduling appointments,” Berrell says. Others feared that older patients were less tech savvy and would have difficulty accessing their virtual visits. In response, team members posted informational fliers in exam rooms and emailed instructions to patients before their appointments.
Building team engagement
Key to the team’s success was engaging everyone, including physicians. Medical assistants and nurses partnered with providers to review physician schedules and flag appointments they could convert to virtual visits.
Also, UBT members participated in weekly huddles “where we brainstormed new tests of change and talked about what worked and what didn’t work,” says Maddox. The team’s efforts paid off.
Patient satisfaction scores for ease of scheduling appointments jumped from 53% to 85% between August 2019 and December 2020. And because members access video visits through kp.org, website registration among the department’s patients increased by nearly 10% during the past year.
The hard work has not gone unnoticed. This past fall, the team received the region’s UBT Excellence Recognition Award for improving service and access.
Maddox attributes the team’s success to strong relationships rooted in partnership. “We know that we would not have had this success if our team didn’t work together.”
(plain node.html.twig - needs theming)
( still node.html.twig ... )
- Taking “voice of the customer” training, which advocates direct input from clients to improve a process or service
- Shadowing nurses to better understand their perspective and identify the root causes of complaints about late or missing medication
- Starting the morning shift 30 minutes earlier to ensure timely delivery of medications
What can your team do to listen to the voice of your customers? Especially if those customers are fellow employees in a different department?
( end node.html.twig ... )
How Unit-Based Teams Make Kaiser Permanente a Better Place to Work
Deck
Positive results for KP members, patients and workers
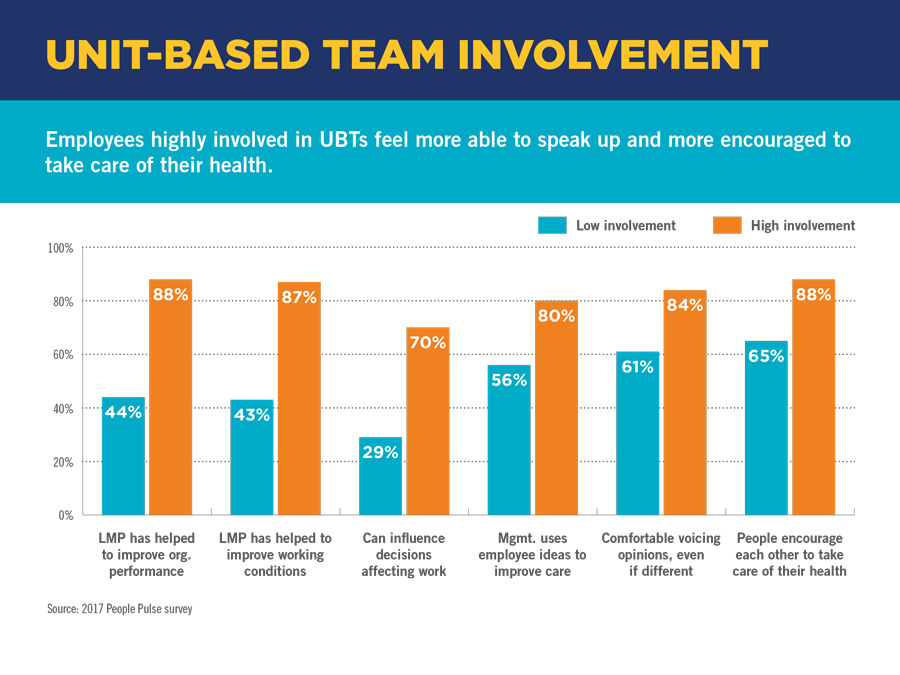
Do teams get better results when frontline workers are engaged, free to speak and can influence decisions? Yes, say the people who know best — Kaiser Permanente workers and managers themselves.
Recent People Pulse surveys confirm that unit-based teams get positive results for health plan members and patients, the organization and workers themselves.
For instance, the 2017 People Pulse survey of more than 155,000 KP employees showed that when union-represented employees are highly involved in UBT activities, they get 29 percent higher scores on measures of their willingness to speak up — a key driver of patient and workplace safety and satisfaction. They also get 33 percent higher scores on questions regarding workplace health and wellness.
Improved safety and satisfaction
Further analysis, included in the 2016 People Pulse survey, showed that teams with high employee involvement have:
- 18 percent fewer workplace injuries
- 13 percent fewer lost work days
- 4 percent higher patient satisfaction
“Our findings show that employees who are highly involved in their unit-based teams feel more able to speak up and more encouraged to take care of their health,” says Nicole VanderHorst, principal research consultant with KP Engagement & Inclusion Analytics. “That makes them more likely to have better performance outcomes.”
A better way to work
Workers’ greater propensity to speak up and look after their health when they’re involved in team activities covers several questions (see chart below). For example, workers who are highly involved in their UBTs are far more likely to say:
- The Labor Management Partnership has helped improve organizational performance and working conditions.
- They can influence decisions affecting their work.
- They’re comfortable voicing differing opinions.
- Management uses their ideas to improve care.
- They’re encouraged, and encourage others, to take care of their health.
Roots of workforce engagement
All these factors contribute to a better employee experience as well as performance. And UBTs reflect KP’s unique history with the labor movement.
“Henry Kaiser was perhaps the 20th century’s most worker-friendly industrialist. He supported organized labor and knew that people step up when allowed to exert their job experience, as they do with UBTs,” says KP archivist and historian Lincoln Cushing. “He trusted employees to make decisions that benefitted themselves and their organizations.”
If you belong to a unit-based team — and most union-represented employees do — talk with a team co-lead about ways to get more involved.
Listening Is Key for Audiology Co-Leads
Deck
Appreciating each other’s different skills and background helps relationship sing
“You have two ears and one mouth for a reason,” television’s Judge Judy frequently says, quoting an ancient Greek philosopher. “You should listen twice as much as you talk.” Successful co-leads realize that making a partnership work requires listening and learning from one another.
Caroline Masikonde, RN, had been a management co-lead with the urgent care team at Largo Medical Center in the Mid-Atlantic States, an experience that helped her understand the importance of valuing her partner’s input. But when she accepted a new role as clinical operations manager in Northern Virginia Audiology in January 2016, she didn’t have any experience in audiology. So she’s relied heavily on her new labor co-lead, Lynn M. Reese, Au.D., a UFCW Local 400 member. Masikonde has learned why audiology UBT members escort patients outside (so they can try out new hearing aids in different conditions)—and her willingness to listen helped the co-leads bond quickly.
“Lynn is very experienced,” says Masikonde. “I lean on her even now.”
Reese, on the other hand, was new to the unit-based team structure, since the audiology UBT had just formed. That’s where Masikonde’s expertise came in. “We fit together pretty well,” says Reese. “Caroline is very open to listening and learning new things.”
Reese, too, expanded her knowledge, growing into an appreciation that she and Masikonde have equal say on what’s now a Level 4 UBT. “Everyone contributes,” says Reese. The ability to speak up led to Reese and the rest of the team requesting and receiving approval for an additional booth to test patients’ hearing.
Relationship tested
Their new relationship was tested when a member—after waiting more than 12 weeks for a refund on a hearing aid that had cost more than $1,000—alerted them, loudly and angrily, to the problem.
Instead of pointing fingers, UBT members figured out the issue: The refund request had to be processed through a department in Southern California, but the team had no way to follow up once the request was submitted.
“This lady forced us to look at this and do better for our members,” Masikonde says. “It prompted us to come up with a better workflow,” and now the team has names and contact information for the people who work on the refunds.
“Even though it was a bad situation, she made us want to improve,” Reese says.
Because the co-leads already were accustomed to relying on and listening to each other, they were able to quickly and calmly handle this tense situation with the unhappy member.
“We really learned our lesson,” Masikonde says. “Recently, we did a refund on a Monday—and by Friday, the member had the check. Lynn and I know our parts and do our dance.”
(plain node.html.twig - needs theming)
( still node.html.twig ... )
- Involving the entire team in the promotion to sign up members to kp.org
- Posting signs at every location to encourage registration, and speaking with patients during appointments
- Speaking directly with members to tout the benefits of kp.org
What can your team do to encourage patients and members to sign up on kp.org?
( end node.html.twig ... )
(plain node.html.twig - needs theming)
( still node.html.twig ... )
- Following the successful practice of another team that solved the same problem
- Offering kid-friendly food like peanut butter and jelly sandwiches
- Creating restaurant style menus with imagery of zoo animals
What can your team do to listen to the voice of the patient? And how could your team learn from other teams that have tackled challenges similar to yours?
( end node.html.twig ... )
(plain node.html.twig - needs theming)
( still node.html.twig ... )
- Creating a "tick sheet" for staff to note how much paper and toner is wasted
- Figuring how often IT is called and how many patients are affected
- Getting authorization for newer and more efficient printers
What can your team do to build a business case for better equipment? What else could your team do to reduce wasted time and effort?
( end node.html.twig ... )
(plain node.html.twig - needs theming)
( still node.html.twig ... )
- Using a checklist of important topics as a teaching tool for new parents at discharge with their new baby
- Speaking with them at a time when they are most likely to understand and take in the information
- Creating a script for nurses that doesn't feel rehearsed or fake
What can your team do to improve your communication with patients?
( end node.html.twig ... )
(plain node.html.twig - needs theming)
( still node.html.twig ... )
The KP Value Compass commits us to delivering the best quality and service at the most affordable price, in the best place to work. And here’s the thing about service—everybody knows how to tell bad from good and good from great.
It’s not easy, in the crunch of a busy workday, to give every member and patient great service every time they call or visit. But these three simple tools can help. Each can be learned quickly and can be discussed, used and perfected by your team:
( end node.html.twig ... )
(plain node.html.twig - needs theming)
( still node.html.twig ... )
- Making phone calls to help make appointments and answer questions
- Creating a "road map" on how to navigate Kaiser Permanente and utilize services
- Greeting new members when they come in and provide useful information
What can your team do to welcome new members? And what could your team do to leverage its members' unique strengths and knowledge?